D. T. Masson Tumor
Name of patient
Disease type

Personal story
Mrs. T, 39 years old, is a mother of two underaged children, academically educated and sport-active without a history of any underlying serious disease.
In January 2022, the patient noticed a blue round shaped pigmentation at skin level on the distal thigh, approximately 1 cm in diameter, resembling hematoma.
Since the lesion was persisting the patient made an appointment at the local dermatologist, who suggested a diagnosis of small hemangioma. No therapy was prescribed.
In March 2022, the patient noticed a change in the lesion’s appearance with newly developed skin elevation and swelling, thinning of the overlying skin, and rapid growth, measuring 2 cm. Due to growing anxiety, the patient arranged one more appointment in the same dermatological practice. On this occasion, and because of the worrisome characteristics, the dermatologist recommended excision by a surgeon.
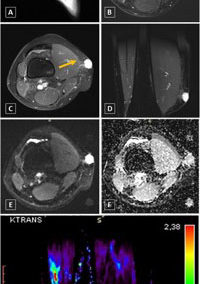
Sonography showed a well demarcated hypoechogenic lesion in the subcutaneous tissue with thickening of the adjacent fascia and hypervascularization on Doppler examination. The differential diagnosis included dermatofibrosarcoma protuberans. MRI with additional dynamic contrast-enhanced sequence revealed an irregular hypervascular soft tissue lesion with pathological contrast enhancement of the surrounding subcutaneous soft tissue, highly suspicious for sarcoma. Considering the potential malignancy, an ultrasound guided biopsy was performed on the following day.
The patient was sent to an oncological-orthopedic out-patient centre for further management depending on the histological outcome.
The histological result showed an intravascular lesion corresponding to an intravascular papillary endothelial hyperplasia or Masson tumor without any signs of malignancy in the biopsy specimens.
An interdisciplinary board decided that the lesion needed to be resected including the fascia of the musculus vastus lateralis, being aware that only a R1-resection type could be achieved with the possibility of a follow-up resection in case of malignancy.
The resection of the lesion should be performed within 10 days.
Radiological Findings
Masson Tumor, also known as intravascular papillary endothelial hyperplasia (IPEH), is a rare vascular lesion of the skin or subcutaneous tissues. It is characterized by benign, reactive, proliferation of endothelial cells within the vascular lumen associated with organized thrombus (1). The importance of a Masson tumor lies in its ability to mimic a malignant neoplasm such as angiosarcoma, thus posing a diagnostic challenge.
Masson tumor is classified into primary and secondary form. Primary IPEH occurs in dilated vascular spaces in the superficial soft tissues of the digits or head and neck (2, 3). Secondary IPEH develops within a pre-existing vascular lesion, usually within a hemangioma or vascular malformation (1). Simple excision is usually curative in both cases, especially for the primary IPEH.
Ultrasound usually shows superficially located, ovoid or round soft tissue lesion with peripheral and varying central vascularity, as shown in our case (figure -2).
MRI, especially in case of primary IPEH, demonstrates peripheral intermediate T1-weighted signal and hyperintense signal on T2-weighted image with varying degrees of central nodular heterogeneity. Contrast enhanced T1-weighted image shows peripheral enhancement with varying degrees of central enhancement. Morphologically, this reflects a nature of the lesion with a combination of the internal organized thrombus (heterogenousT2 signal and absent enhancement, centrally) and intravascular proliferation (high T2-signal and rapid enhancement, seen peripherally) (4, 5).
To conclude, the radiological findings usually indicate the vascular nature of the lesion, but it is diagnostically challenging to differentiate IPEH from other malignant vascular neoplasms (6, 7). Therefore, these lesions still require biopsy for histological confirmation of the diagnosis.
Authors: Mira Feichtinger, MD and Jasminka Igrec MD, PhD, Department of Radiology, Medical University of Graz, Graz, Austria. [email protected]
References
- Weiss SW, Goldblum JR. Enzinger & Weiss`s soft tissue tumors Philadelphia: Mosby; 2008. p. 633-79
- Clearkin KP, Enzinger FM. Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976; 100 (8):441-4
- Hashimont H, Daimaru Y, Enjoji M. Intravascular papillary endothelial hyperplasia. a clinicopathologic study of 91 cases. Am J Dermatopathol. 1983; 5(6):539-46.
- Kitagawa Y, Tamai K, Kim Y, Hayashi M, Makino A, Takai S. Intravascular papillary endothelial hyperplasia of the digit: MRI feautures with pathological correlation. J Hand Surg Eur Vol. 2013;38(3):306-12
- Lee SJ, Choo HJ, Park JS, Park YM, Eun CK, Hong SH, et al. Imaging findings of intravascular papillary endothelial hyperplasia presenting in extremities: correlation with pathological findings. Skeletal Radiol. 2010; 39(8):783-9.
- Salyer WR, Salyer DC (1975)Intravascular angiomatosis: development and distinction from angiosarcoma. Cancer. 36(3):995-1001
- Samadi K, Salazar GM. (2019) Role of imaging in the diagnosis of vascular malformations. Cardiovasc Diagn Ther. Aug;9(Suppl 1): S143-S151