Bianca S. Tenosynovial giant cell tumor of the joint with diffuse subtype
Name of patient
Disease type

Personal story
At the first clinical presentation, Ms. S. was a previously healthy 17-year-old woman in December 2016. She played soccer at her local recreational park with friends of the same age as she usually did. However, after sportive activity without any trauma, she developed painful swelling of her left knee joint. Due to the missing trauma history, she went to the local hospital specialized in trauma-orthopedic surgery to get a thorough check-up.
After conventional radiographs, no bone-related injury was identified, and she underwent an MRI scan to check for meniscal damage. Unfortunately, this MRI was the beginning of a long-lasting painful journey.
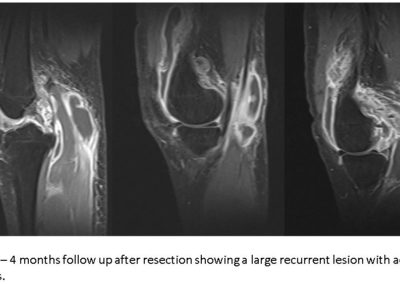
The initial MRI examination identified a suspicious nodular soft tissue lesion of the joint suggestive of a giant cell tumor of the joint (GCTJ) (Figure 1). Arthroscopic resection was performed three weeks after the first MRI exam, and the histological specimen confirmed the working diagnosis of GCTJ with the rare diffuse subtype.
Four months after resection, the checkup MRI showed large recurrent formations of the benign tumor within the left knee joint (Figure 2). She was still experiencing frequent pain sensations up to 8 on a scale of 10 with a noticeable reduction of quality of life due to missing sports and decreased movement ability in general.
Within the next several months, she underwent frequent MRI check-ups with growing tumor formation and recurring resections, radiation therapy, and medication with ongoing pain throughout her daily life.
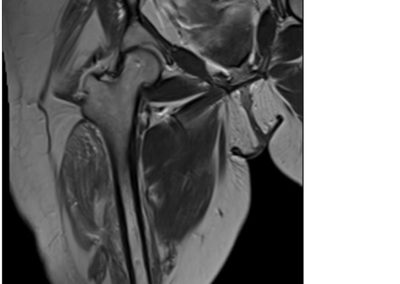
42 months after initial presentation at the trauma hospital, amputation of her left limb was performed due to the inability to get the local recurrence of this aggressive yet benign tumor under control. It was a tough decision for all involved clinicians and radiologists who did the regular checkup, but since June 2020, she has been disease-free with a good quality of life (Figure 3).
Radiological Findings
Tendosynovial giant cell tumor is a rare, usually benign neoplastic proliferation of synovial cells of the joints, burse, or tendons, mostly affecting early to middle age patients between the 2nd to 4th decade. It rarely metastazies lymphogenic. Typically, tenosynovial giant cell tumor of the joint is a monoarticular condition, although, in the pediatric population it can occur polyarticular. There is a slight female prevalence.
Computed tomography (CT) and radiographic features are nonspecific and include soft tissue swelling due to extraarticular soft tissue masses and, in advanced cases, pressure erosions of the underlying bone.
The primary diagnostic imaging modality for diagnosis and follow-up is MR imaging.
MRI features are, in most cases, specific with a limited differential diagnostic potential. These lesions are commonly demonstrated as localized nodules, in case of localized form, or diffuse synovial thickening, in diffuse form with low signal intensity on T1-weighted and T2-weighted sequences and moderate enhancement. Susceptibility artifacts (“blooming”) on gradient echo – and susceptibility weighted images result from hemosiderin accumulation, a pathognomonic finding for definitive diagnosis. After application of Gadolinium contrast giant cell tumor of the joint shows moderate contrast enhancement.
Author: Jakob Steiner, MD, Department of Radiology, Medical University of Graz, Graz, Austria. [email protected]
References
- Ehrenstein V, Andersen SL, Qazi I, Sankar N, Pedersen AB, Sikorski R, Acquavella JF. Tenosynovial Giant Cell Tumor: Incidence, Prevalence, Patient Characteristics, and Recurrence. A Registry-based Cohort Study in Denmark. J Rheumatol. 2017 Oct;44(10):1476-1483. doi: 10.3899/jrheum.160816. Epub 2017 Aug 1. PMID: 28765257.
- Kalil RK, Unni KK. Malignancy in pigmented villonodular synovitis. Skeletal Radiol 1998;27: 392–395.
- Hughes, T. H., Sartoris, D. J., Schweitzer, M. E., & Resnick, D. L. (1995). Pigmented villonodular synovitis: MRI characteristics. Skeletal Radiology, 24(1), 7–12.
- Horger M, Vogel M, Schmit M, Wehrmann M. Imaging in pigmented villonodular synovitis [German]. Röfo 2007;179:97–99.