Mr. Humulus Recurrent basilar artery occlusion
Name of patient
Disease type
Personal story
Mr. Humulus, a middle-aged man, presented with acute onset of dizziness, left-sided hemiparesis and progressive loss of consciousness. One month earlier, he had suffered from a bi-thalamic infarct treated with intravenous thrombolysis (IVT) and recovered well. His vascular risk factors included dyslipidemia, coronary heart disease and peripheral artery disease.
CT angiography (CTA) revealed basilar artery occlusion (BAO) and additionally showed a calcified hypoplastic right vertebral artery with multifocal stenoses. IVT and mechanical thrombectomy (MT) achieved complete recanalization and an excellent neurological outcome. Nine days post-thrombectomy, while still in hospital, Mr. Humulus suddenly developed acute left-sided hemiparesis and dysarthria. MR angiography (MRA) showed distal BAO; subsequently we performed direct MT.
Again, full recanalization was achieved and he remarkably improved. Two weeks later, Mr. Humulus was discharged without any neurological deficits but was readmitted only four days after discharge with left-sided hemiparesis and dysarthria. CTA confirmed the third recurrent BAO, and the vessel was again successfully recanalized with MT. Despite multiple small infarcts, Mr. Humulus had a very good clinical outcome and was discharged after further stroke work-up and early rehabilitation.
One week after discharge, Mr. Humulus again presented with vertigo and left-sided sensory deficits. “I know what´s going on. I´m having a basilar thrombosis again!” he explained to the nurses and doctors while entering the emergency room with a smile. MRA revealed the fourth recurrent BAO within weeks, which was again treated by endovascular therapy.
Radiological Findings
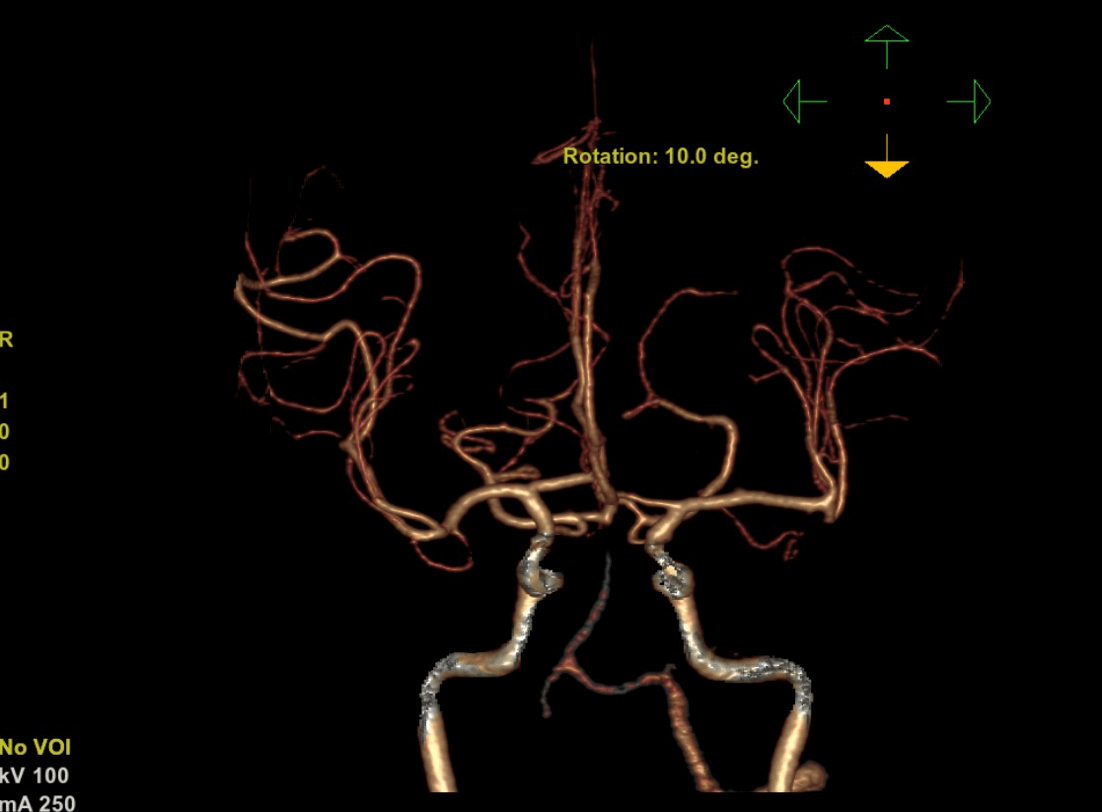
Despite extensive stroke-workup and different anticoagulation therapy regiments Mr. Humulus developed four recurrent BAOs during a remarkably short time period. Radiology not only helped to identify and treat this life-threatening condition, but also to identify a dysplastic right vertebral artery, which was an important differential diagnosis regarding the cause of recurrent ischemia in the posterior circulation. Because this embolic source could not be controlled by conservative treatment strategies, we performed a successful coil embolization of the distal right vertebral artery.
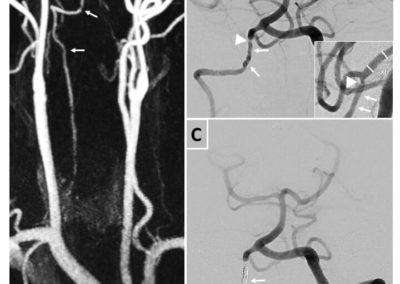
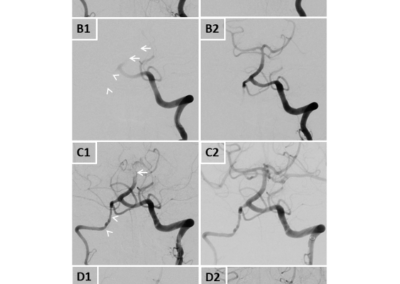
Figure 1 shows digital subtraction angiography (DSA) images of all four BAOs pre (A1,B1,C1,D1) and post interventional (A2,B2,C2,D2). Arrows display arterial occlusion and / or thrombi, arrowheads display a hypoplastic and dysplastic right vertebral artery.
Figure 2A shows MRA images of the right irregular shaped vertebral artery with multiple intra- and extra cranial irregularities (tailed arrows) corresponding to the diagnosis of a dysplastic vertebral artery. Figure 2B shows pre interventional DSA of the posterior circulation with irregularities (tailed arrows) and distal stenosis of the vertebral artery (arrowhead) in two plains. Figure 2C shows post interventional DSA of the posterior circulation after coil occlusion of the distal right vertebral artery (tailed arrow).
Regarding the stenotic right vertebral artery, our patient’s history of coronary heart and peripheral artery diseases suggest an atherosclerotic cause as source of recurrent embolism. However, unsuccessful antiplatelet and anticoagulation therapy suggests a non-atherosclerotic mechanism, such as focal fibromuscular dysplasia. After final therapy, Mr. Humulus had no persisting neurological deficits and until today, more than 2 years after his last stroke, no further cerebrovascular events occurred.
Authors:
Stefan L. Leber MD, Division of Neuroradiology, Vascular and Interventional Radiology, Department of Radiology, Medical University of Graz, Graz, Austria.
[email protected]
References
Leber SL, Fandler-Höfler S, Kneihsl M, Augustin M, Deutschmann H, Gattringer T. Case Report: Four Early Recurrent Basilar Artery Occlusions Successfully Treated With Mechanical Thrombectomy and Subsequent Vertebral Artery Coil Occlusion. Front Neurol. 2021;12:698488. Published 2021 Sep 20. doi:10.3389/fneur.2021.698488