Erik Briers Prostate Cancer
Name of patient
Disease type

Personal story
Erik is retired and lives in Belgium. In 2001 at age 50 a routine checkup included a PSA test. The test resulted in a value of 5,3ng/mL which is too high if compared to what is considered “normal” for that age.
After confirmation, biopsies followed and consultation with a urologist. In six months, a PSA value above 20ng/mL and positive biopsies were detected.
Since these results are classified as high-risk (D’Amico), active treatment was started and on January 2, 2002, the prostate cancer was removed surgically.
Today Erik has taken care of the major side effects and is in excellent health. He enjoys life and his three grandsons which he would never have met if his cancer were to be found late.
In the twenty years since his diagnosis science has evolved and consensus on early detection of prostate cancer is growing. Today we can safely advice men to inform themselves on prostate cancer which will “hit” one in seven men. Well informed they can then enter a risk based early detection protocol with a PSA test.
If the PSA test reveals the presence of a prostate cancer “risk”, the man will be referred to a urologist to have an MRI of the prostate. Based on the results of the MRI the man can have a trans perineal biopsy directed mostly to the suspicious areas in the prostate.
Using MRI prevents unnecessary biopsies, and analysis of the biopsies will make it possible to offer an optimal treatment if positive. Treatments can be active surveillance or an active treatment.
The objective is to find prostate cancer with intermediary or high risk and to treat them curatively. Detecting prostate cancer in a late stage will cause loss of quality of life, bad prognosis and (very) high cost to the health care system.
Radiological Findings
Prostate cancer is suspected based on an elevated PSA level or an abnormal DRE. Most international guidelines now recommend that patients with suspected prostate cancer undergo a multiparametric MRI of the prostate.
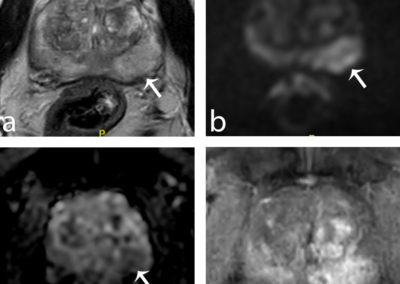
Prostate MRI is called “multiparametric” because it combines several “pulse sequences”, i.e. several ways of looking at the prostate with MRI: T2-weighted imaging, diffusion-weighted imaging, dynamic contrast-enhanced imaging. Each abnormalities seen is assigned a so-called “PI-RADS score” that depends on its appearance on each sequence. This score ranges from 1 to 5 and assesses the risk that the lesion is an aggressive cancer (1: aggressive cancer highly unlikely; 5: aggressive cancer highly likely).
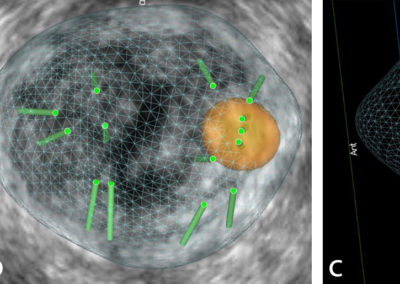
The confirmation of the nature of the lesions seen on MRI is obtained by prostate biopsy. Usually “systematic” samples (that are obtained at predefined locations in the gland) are combined with “targeted” samples (that are directed to the lesions seen on MRI with a PI-RADS score ≥3). Ideally, targeted samples are obtained after software fusion of MR images and transrectal US images to make sure that they sample the lesion correctly.
This technique has an excellent sensitivity (approximately 90%) for detecting aggressive cancers.
Figure 1: Multiparametric MRI showing a suspicious lesion for cancer with a PI-RADS score of 5 (arrows; a: T2-weighted imaging; b: diffusion-weighted imaging; c: diffusion-weighted imaging; d: dynamic contrast-enhanced imaging)
Figure 2: Systematic and targeted biopsy performed under MR/ultrasound elastic fusion. First, the prostate is outlined on MR images and the position of the lesion noted (a, orange circle). Then, the biopsy is performed under MR/ultrasound fusion. The fusion allows to project the position of the target (b-c, orange sphere) and biopsy samples (b-c, green tubes) within the 3D ultrasound volume (b, axial projection; c, sagittal projection). Note the three targeted samples obtained in the center of the lesion.
Prof. Olivier Rouvière
References
EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer N. Mottet (Chair) et al. ©European Association of Urology 2022