Ms L. Treatment of a sciatica by CT‑guided epidural injection
Name of patient
Disease type

Personal story
Ms L. is 25-years-old, single and a nursing assistant in a public hospital.
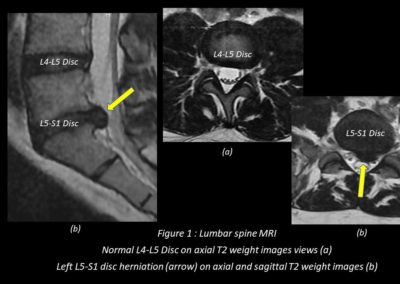
After lifting a patient to use the toilet during her work in January 2019, she developed disabling lower back pain; a first MRI performed showed a L5-S1 disk herniation lateralized on the left side (Figure 1). Everything was back in order after 3 weeks of medical treatment and 15-days of work stoppage.
In November 2021, she suddenly presented a new and violent left lumbosciatica (neuralgic pain descending into her buttock, then along the calf to the foot in front of the left fifth toe).
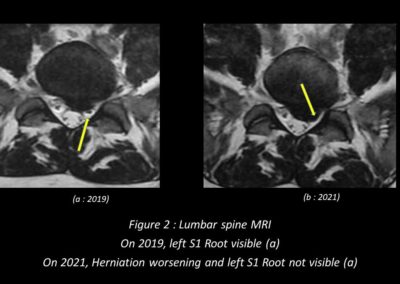
With a complete inability to move, she stayed at home for 4 long weeks during which different treatments were tried with more or less success: a new work stoppage, analgesics, anti-inflammatories, corticosteroids. A new MRI scan showed a worsening of the L5-S1 Herniated Disk and a left S1 nerve mass effect (Figure 2).
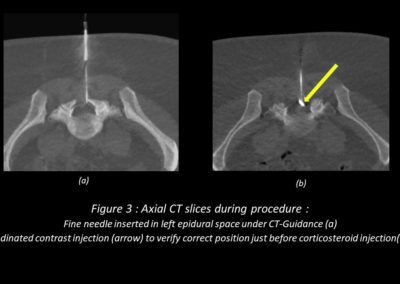
After a consultation with a specialised radiologist (necessary to check possible precautions to be taken, detect any contraindications and explain how the gesture happens, what can be expected in terms of risk and results), he practiced, on an outpatient basis a few days later, a local injection of powerful corticosteroids under CT-guidance.
She was placed in a prone position (Figure3) on the scanner table. After the CT scan of the affected level, asepsis and local anaesthesia, a thin needle was placed posteriorly in the epidural fatty space on the side of the conflicted area (Figure 4a). The injection of a few cc of iodinated contrast, check the absence of vascular passage, avoid dural sac perforation and secure the injection of the local corticosteroid (Figure 4b).
She felt improvement after 24 hours, was able to reduce the doses of oral analgesics after 8 days and was back to work and living normally after 15 days.
Radiological Findings
Low back pain is a major source of disability worldwide, estimates on the lifetime prevalence of LBP generally range between 50% and 80% (1,2).
Plain X-rays, CT and MRI are the most useful first-line imaging means in patients complaining of low back pain or sciatica.
Medical imaging is necessary to look for non-degenerative causes of these pains: primary bone tumours, vertebral metastases, infections (spondylodiscitis), compaction-fractures (osteoporosis), metabolic or rheumatological pathologies (spondyloarthropathy, rheumatoid arthritis) (3). In the majority of cases the origin of these pains is degenerative, the disc-vertebra complex, being considered as a joint like the knee or hip deteriorates over time; these are osteoarthritis narrowing of the lumbar canal, posterior arthropathies and especially disc degeneration which is the most common cause of lumbar neuralgia.
MRI (like CT) is used to diagnose and study the anatomy of a herniated lumbar disc and its possible nervous impact (4) (Figures 1 and 2). It is the inflammatory reaction around the displaced disc fragment that causes the pain (2).
The treatment is primarily medical (analgesics, non-steroid or steroid anti-inflammatory drugs, opioids, physiotherapy) allowing in the vast majority of cases to solve the problem. Local infiltration of corticosteroids may be proposed in case of ineffectiveness or incomplete efficacy after well-conducted medical treatment. They are most often carried out under CT-guidance. The last resort is surgical (percutaneous discectomy or surgical).
Results on pain are good in 60-80% immediately or delayed (5,6,7). They allow a reduction in surgical indications of 10%.
Adverse events and complications are rare (transient reactivation of pain, hypertensive flare-up, allergic reaction, vaso-vagal reaction, epidural hematoma, infection, diabetic decompensation, neurological spinal cord injury, neurologic damage) and can be avoided if the indications are well established and all procedural precautions taken (8,9).
D.Carrié
French Radiologist, MD.
References
- P Cohen and al. Effect of MRI on Treatment Results or Decision Making in Patients With Lumbosacral Radiculopathy Referred for Epidural Steroid Injections A Multicenter, Randomized Controlled Trial Steven
Arch Intern Med. 2012;172(2):134-142. - Y. Ota and al. Mechanisms and Origins of Spinal Pain: from Molecules to Anatomy, with Diagnostic Clues and Imaging
RadioGraphics 2020; 40:1163–1181 - EB. Smith Oh, My Aching Back! A Review of Spinal Arthropathies
RadioGraphics 2016; 36:935–936 - CWA Pfirrmann MR Image–based grading of lumbar nerve root Compromise due to Disk Herniation : reliability study with surgical correlation
Radiology 2004; 230:583–588 - KD Riew and al. Nerve root blocks in the treatment of lumbar radicular pain: a minimum 5-year follow-up. J Bone Joint Surg Am 2006;88:1722–1725.
- MD Fritz and al. Management of Chronic Low Back Pain: Rationales, Prin ciples, and Targets of Imaging-guided Spinal Injection Diagnosis
RadioGraphics 2007; 27:1751–1771 - A. Gangi and al. Interventional Musculoskeletal Procedures
Radiographics https://doi.org/10.1148/radiographics.21.2.g01mre1e1 - WE Palmer and al. Spinal Injections for Pain Management
Radiology 2016; 281:669–688 - I Pountos and al. Safety of Epidural Corticosteroid Injections
Drugs R D (2016) 16:19–34